Program Description Paper
from Bartos et al.
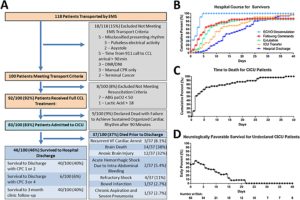
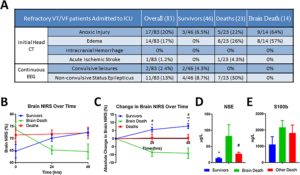
Of 100 appropriately transported patients, 83 achieved CICU admission. 40/83 (48%) discharged functionally intact. Multi-system organ failure occurred in all patients. Cardiac, pulmonary, renal, and liver injury improved within 3–4 days. Neurologic injury caused death in 26/37 (70%) patients. Poor neurologic outcomes were associated with anoxic injury or cerebral edema on admission head CT, decline in cerebral oximetry over the first 48 h, and elevated neuron specific enolase on CICU admission. For survivors, mean time to ECMO decannulation was 3.5 ± 0.2 days, following commands at 5.7 ± 0.8 days, and hospital discharge at 21 ± 3.2 days. 41/83 (49%) patients developed infections. CPR caused traumatic injury requiring procedural/surgical intervention in 22/83 (27%) patients.
Inclusion Criteria
Prehospital
- age 18–75 years
- OHCA of presumed cardiac etiology
- initial cardiac arrest rhythm of VF/VT
- received 3 direct current shocks without ROSC
- received Amiodarone 300 mg
- body habitus accommodating a Lund University Cardiac Arrest System (LUCAS®) automated CPR device
- estimated transfer time to the hospital <30 min
In-Hospital
Excluded if:
- end-tidal CO2 < 10 mmHg
- PaO2 < 50 mmHg
- lactic acid >18 mmol/L
- time from EMS activation to CCL arrival >90 min.
If after ECMO, the patient did not regain an organized heart rhythm within the 1st 90 minutes, ECMO was discontinued and support withdrawl
Timings
| Time, mean (SEM), min | 911 to first responder | 7.6 (1.2) |
|---|---|---|
| 911 to CCL arrival | 56.7 (1.8) | |
| CCL arrival to ECMO support | 8 (0.5) |
All patients received a right radial arterial line and an intravascular cooling catheter (Thermogard XP, Zoll).
All patients had diagnostic coronary angio to r/o cardiac etiology of arrest
All patients got a Pan-Scan after the Cath Lab
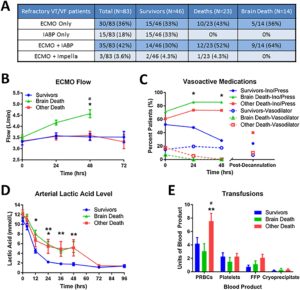
All patients received therapeutic hypothermia (TH) for 24 h. Goal temperature was 34 °C with increases to 35–36 °C if significant bleeding occurred. Patients were maintained in 30-degree reverse trendelenburg with the head midline. Continuous electroencephalogram and cerebral oximetry via near infrared spectroscopy (NIRS; Equanox; Nonin) were initiated within 24 h. Hemodynamics were maintained with mechanical, inotrope, pressor, and vasodilator support with goal mean arterial pressure (MAP) between 65 and 100 mmHg. ECMO flow was maximized until pressors were discontinued, then reduced, as tolerated, promoting native cardiac function. ECMO decannulation readiness was assessed daily with short weaning trials and simultaneous echocardiography. On ECMO, rest ventilator settings were used with 7–10 cmH2O positive end-expiratory pressure at 12 breaths per minute, and tidal volumes of 6–8 mL/kg ideal body weight. Plateau pressures were maintained below 30 cmH2O. Settings were adjusted after ECMO decannulation. Continuous veno-venous hemodialysis was provided when needed. Potassium was replaced up to 3.0 mmol/L during TH and 4.0 mmol/L once rewarmed. Enteral nutrition was provided via oral-gastric (OG) or nasal-gastric (NG) access once rewarmed. All patients received five days of empiric, broad-spectrum antibiotics with narrowed coverage thereafter, as necessary. Daily surveillance blood cultures were performed while on ECMO. Blood products were provided with a goal hemoglobin >8 g/dL, platelets >100,000 per μL, and fibrinogen >200 mg/dL. Heparin maintained activated clotting time (ACT) 180–200 s while on ECMO. For life-threatening bleeding, the ACT goal was reduced as low as 140–160 s. All PCI patients received aspirin 81 mg and ticagrelor by NG or OG tube.
Distal Perfusion Cath
Arrow Mac Cath (9F) placed in the lab
Of the 37 patients who died prior to hospital discharge, mean time to death was 7.4 ± 1.5 days (Fig. 1C). Catastrophic neurologic injury caused death for 26/37 (70%) patients. Brain Death accounted for 14/37 [38%] deaths and anoxic brain injury accounted for 12/37 (32%) deaths. Non-neurologic causes included recurrent refractory VF (3/37), acute hemorrhagic shock (2/37), refractory vasoplegic shock (4/37), bowel infarction (1/37), and severe chronic aspiration pneumonia (1/37) (Fig. 1A).
End-organ dysfunction
Left ventricular function was severely compromised in all patients for the first 48 h requiring continued ECMO/IABP support (Fig. 4A). Significant recovery was observed within 5 days. Mean left ventricular ejection fraction was 15.3% at 24 h, 28% at 48 h, 37% at 4 days, and 44% at hospital discharge
Trauma
Prolonged CPR caused substantial trauma: 27/83 (33%) had rib fractures, 6/83 (7%) had pneumothorax, 2/83 (2%) required a chest tube, 8/83 (11%) had intra-thoracic bleeding, 1/83 (1%) had hemopericardium due to a ruptured right ventricle, and 5/83 (6%) had intra-peritoneal bleeding. Traumatic injury required urgent or emergent procedural/surgical intervention in 22/83 (27%) patients including 14/40 (35%) functionally intact survivors. Throughout hospitalization, 36/83 (43%) patients including 23/46 (50%) Survivors required an invasive/surgical procedure. Complications, procedures, and patient outcome are shown in Table 2.
Several unique features of the CICU care deserve attention. All patients were considered viable and eligible for any necessary intervention or surgery until definitive declaration of death. This approach allowed determination of an achievable functionally intact survival rate without confounding of physician-advocated early withdrawal of life sustaining therapy.
Neurologic prognostication began no earlier than 72 h following normothermia unless evidence of brain death was present [13,17]. After 72 h, all prognostic factors and family wishes were used to inform decision-making. Nonetheless, only 52% of survivors were following commands within 5 days. The last patient surviving functionally intact began following commands at 22 days. Thus, more than 72 h of comprehensive support was necessary to capture all survivors.