PEA In the Field
PEA OOH Arrest with mean time of 41 minutes low-flow had 23.8% survival to discharge (neuro status not listed in the paper; small study)4
No-Flow Time
Initial rhythm shockable is a surrogate for no-flow time < 10 minutes5
but not so great for less than 10 minutes [10.1136/emermed-2021-211823]
Favorable outcome can still be seen up to 20 minutes of no-flow
Low Flow Time
Debaty G, Resuscitation. 2017 Mar;112:1-10. doi: 10.1016/j.resuscitation.2016.12.011.
- 6 lactate in non-survivors
- 55 vs 65 minutes
- Bystander CPR did not matter—not that we don’t think it matters
- Gender and age did not seem to matter—selection criteria probably trumps (comorbidities)
- Sign of life trumps all
: Haas NL, Coute RA, Hsu CH, Cranford JA, Neumar RW. Descriptive analysis of
extracorporeal cardiopulmonary resuscitation following out-of-hospital cardiac
arrest-An ELSO registry study
. Resuscitation. 2017 Oct;119:56-62. doi:
10.1016/j.resuscitation.2017.08.003. Epub 2017 Aug 5. PubMed PMID: .
- No age difference when stratified by decades of life
While low-flow >30 minutes (37 to be precise) had rare survival in prior studies in non-ecpr patients, this can’t be extended to ecpr patients. Even in non-ecpr trials, this time cut-off does not seem to hold.6,7
41 of 135 patients with a mean cpr time of 55.7 min had d/c with good neuro outcome (In-hosp arrest)8
17.7% of survival with CPR > 60 min9
Fjolner et al. had a median time of 54 minutes low flow (Acta Anaes Scandi 2017;61:176)
Signs of Life
They are a good parameter [ 10.1097/CCM.0000000000006116 ]
Change in EMS Protocols
Immediate transport of viable ECPR patients would mean much shorter low-flow times. Incidence of Load and Go is 6% of EMS responses.10
Large percentage of survivors met termination of resus rules11
Robert Pyo–Interventional
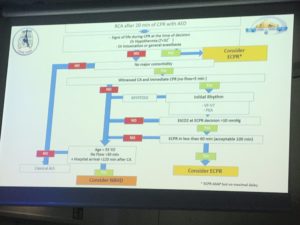
Comparison of Protocols
SAMU
Signs of life trumps all other
No-Flow < 5 OR initial shockable
100 minutes low flow time
Alfred (Exclusion)
- Age> 65
- Unwitnessed arrest
- First checked rhythm is asystole
- > 10 minutes before CPR
- > 45 minutes of CPR prior to commencing cannulation
- Known symptomatic chronic organ failure
- Multiple past coronary revascularizations
- Cirrhosis (jaundice, ascities, encephalopathy)
- ESRF (dialysis)
- Cardiomyopathy (VAD or inotropes)
- Chronic lung disease (NYHA III or IV)
- Chronic pulmonary arterial hypertension
1.
Ahn H, Lee J, Joo K, et al. Point-of-Care Ultrasound-Guided Percutaneous Cannulation of Extracorporeal Membrane Oxygenation: Make it Simple. J Emerg Med. 2018;54(4):507-513. [PubMed]
2.
Voicu S, Henry P, Malissin I, et al. Improving cannulation time for extracorporeal life support in refractory cardiac arrest of presumed cardiac cause – Comparison of two percutaneous cannulation techniques in the catheterization laboratory in a center without on-site cardiovascular surgery. Resuscitation. 2018;122:69-75. [PubMed]
3.
Javaudin F, Leclere B, Segard J, et al. Prognostic performance of early absence of pupillary light reaction after recovery of out of hospital cardiac arrest. Resuscitation. 2018;127:8-13. [PubMed]
4.
Pabst D, Brehm C. Is pulseless electrical activity a reason to refuse cardiopulmonary resuscitation with ECMO support? Am J Emerg Med. 2018;36(4):637-640. [PubMed]
5.
Tanguay-Rioux X, Grunau B, Neumar R, Tallon J, Boone R, Christenson J. Is initial rhythm in OHCA a predictor of preceding no flow time? Implications for bystander response and ECPR candidacy evaluation. Resuscitation. 2018;128:88-92. [PubMed]
6.
Bradley S, Liu W, Chan P, et al. Duration of resuscitation efforts for in-hospital cardiac arrest by predicted outcomes: Insights from Get With The Guidelines – Resuscitation. Resuscitation. 2017;113:128-134. [PubMed]
7.
Goldberger Z, Chan P, Berg R, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380(9852):1473-1481. [PubMed]
8.
Chen Y, Yu H, Huang S, et al. Extracorporeal membrane oxygenation support can extend the duration of cardiopulmonary resuscitation. Crit Care Med. 2008;36(9):2529-2535. [PubMed]
9.
Chen Y, Lin J, Yu H, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372(9638):554-561. [PubMed]
10.
Poppe M, Weiser C, Holzer M, et al. The incidence of “load&go” out-of-hospital cardiac arrest candidates for emergency department utilization of emergency extracorporeal life support: A one-year review. R. 2015;91:131-136. doi:10.1016/j.resuscitation.2015.03.003
11.
Zhang W, Liao J, Liu Z, et al. Out-of-hospital cardiac arrest with Do-Not-Resuscitate orders signed in hospital: Who are the survivors? Resuscitation. 2018;127:68-72. [PubMed]
12.
Leick J, Liebetrau C, Szardien S, et al. Door-to-implantation time of extracorporeal life support systems predicts mortality in patients with out-of-hospital cardiac arrest. Clin Res Cardiol. 2013;102(9):661-669. [PubMed]
13.
Chung M, Shiloh A, Carlese A. Monitoring of the adult patient on venoarterial extracorporeal membrane oxygenation. ScientificWorldJournal. 2014;2014:393258. [PubMed]
14.
Nolan J, Sandroni C. In this patient in refractory cardiac arrest should I continue CPR for longer than 30 min and, if so, how? Intensive Care Med. 2017;43(10):1501-1503. [PubMed]
15.
Hirose H, Pitcher H, Baram M, Cavarocchi N. Issues in the Intensive Care Unit for Patients with Extracorporeal Membrane Oxygenation. Crit Care Clin. 2017;33(4):855-862. [PubMed]
16.
Streitberger K, Leithner C, Wattenberg M, et al. Neuron-Specific Enolase Predicts Poor Outcome After Cardiac Arrest and Targeted Temperature Management: A Multicenter Study on 1,053 Patients. Crit Care Med. 2017;45(7):1145-1151. [PubMed]
CREST Score to predict early decline to ECMO16
Yanno Papers
Early Access to Cath Lab from Minnesota Yanno Paper17 [full text]
Yanno’s Main Paper
ECPR Paper18 [full text]
18 Patients. ECMO was placed in 83%. Seventy‐eight percent of patients had significant coronary artery disease with a high degree of complexity and 67% received PCI. Seventy‐eight percent of patients survived to hospital admission and 55% (10 of 18) survived to hospital discharge, with 50% (9 of 18) achieving good neurological function (cerebral performance categories 1 and 2). No significant ECMO‐related complications were encountered.
MRC refractory VF/VT inclusion criteria (must have all)
-
OHCA with presumed cardiac etiology cardiac arrest.
-
First presenting rhythm was shockable (VF or VT).
-
Age 18 to 75 years.
-
Received at least 3 direct current (DC) shocks without sustained ROSC.
-
Received amiodarone 300 mg.
-
Body could accommodate a Lund University Cardiac Arrest System (LUCAS) automated CPR device.
-
Transfer time from the scene to the CCL of <30 minutes.
Exclusion criteria for early mobilization (presence of 1 would exclude the patient)
-
ROSC before 3 shocks were delivered (transferred to nearest hospital).
-
Nursing home residents.
-
Do Not Resuscitate/Do Not Intubate.
-
Known terminal illness, (eg, cancer, end‐stage liver, kidney, or heart disease)
-
Traumatic arrest
-
Pulseless electrical activity and asystole
-
Significant bleeding
-
Manual CPR as the only option.
Table 2
| Cardiac Arrest Characteristics (18 Patients) | N (%) |
|---|---|
| Arrest location | |
| Home | 7 (39) |
| Public place | 11 (61) |
| Initial cardiac rhythm | |
| VF/VT | 18 (100) |
| Other | 0 |
| Bystander CPR | |
| Yes | 12 (66) |
| No | 6 (33) |
| Times, min | |
| 911 to first responder | 5.8±3.1 |
| 911 to CCL arrival | 60.1±11 |
| CCL arrival—on ECMO | 6.3±2 |
Of the patients on ECMO admitted to the CICU who survived, average time to decannulation was 52±21 hours. All but 3 patients had ongoing CPR upon arrival to the CCL. Two of the 3 patients with pulses were hypotensive and in cardiogenic shock requiring ECMO initiation.
So 15 came to lab still in Arrest
What is CPC survival in these 15?
Is intermittent ROSC a positive predictor
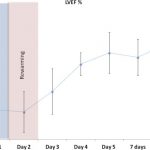
Cardiac function was severely depressed for an average of 3 days, at which point a progressive recovery was observed in the majority of patients continuing until the day of discharge (Figure 3).
JEMS Article from Yanno19
CRITICAL STUDY of ecpr outcome based on 3 factors
initial shockable, time to hospital arrival within 45 minutes, and age <75 years
Favourable neurological outcomes were as follows: patients meeting no or one criterion: 2.3% (1/43), those meeting
two criteria: 8% (13/163), and those meeting all criteria: 16.1% (50/311) (P-value = 0.004).
Conclusions: In this study, approximately 60% of patients treated by ECPR met the three criteria (initial shockable, time to hospital arrival within 45
minutes, and age <75 years), and the greater the number of criteria met, the better were the neurological outcomes achieved.
[10.1016/j.resuscitation.2022.06.007]
A2BCDE3
- 3 Rhythm Checks
- Age < 75
- Activity Signs of Life
- Bystander Witnessed
- CPR within 5 minutes of arrest
- Defibbable (or PEA)
- Endstage disease excluded
- ETCO2 >=10
- Estimated time to ECPR < 60 minutes
- Estimated Complications (for cannulation)
[10.1016/j.resuscitation.2021.12.031]